IMPACT ON HEALTH OUTCOMES
Over the last few years, it has been very clear from research that Social Determinants of Health (SDOH) variables have a major impact on health outcomes. It is estimated that close to 80% of health outcomes are impacted by SDOH. With the rise of population-based risk contracts in both the commercial and government sector, it is essential for both providers and payers to collaborate in the identification of best practices to address these SDOH variables. This is especially relevant as providers such as hospitals assume greater risk in arrangements with plans throughout the country such as Accountable Care Organizations (ACO) and bundled payments.
NATIONAL INTEREST AND PROGRESS
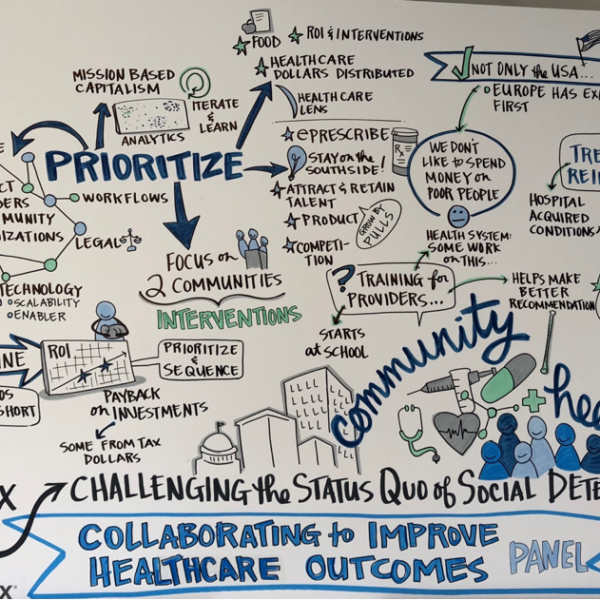
Many national associations such as the American Hospital Association (AHA) and America’s Essential Hospitals have developed resources and launched learning collaboratives for hospitals and health systems to address these variables such as food insecurity, housing, and transportation. Health system innovation and care-redesign models driven by organizations such as Healthbox and AVIA have launched collaboratives and forums to educate and address SDOH initiatives. The May 3, 2018, Healthbox forum discussion on “Challenging the Status Quo of Social Determinants” visually captured the opportunities and challenges ahead into one image (Figure 1):

These variables have always been a focus of many health systems in terms of articulating their benefit to the community, but now they have particular importance given the rise of more population risk contracts.
Several major barriers have impeded the industry’s progress in addressing SDOH variables: funding and regulations. Fortunately, we have begun to see opportunities in both areas emerge in 2018!
MEDICARE UPDATES AND THE BENEFITS OF SOCIAL DETERMINANTS OF HEALTH DATA
Medicare Advantage (MA) has a regulation titled “Uniformity Standard” that requires all of the plan’s benefits, including cost-sharing, be the same for all plan enrollees. On April 2, 2018, the Centers for Medicare & Medicaid Services (CMS) outlined several widespread changes in this regulation that both providers and plans have advocated for over the last several years in their 2019 Medicare Advantage Call Letter. CMS expanded the flexibility of lifting the uniformity of supplemental benefit to allow different segments of an MA plan to offer specific benefits to a targeted population like diabetics. This can begin in CY 2019 (January 1, 2019) after the plan designs are approved by CMS. An example could be reduced cost sharing for foot or eye exams. In their official bids that were submitted by the June 4, 2018 deadline, the MA plans can include any of these supplemental benefit elements. Hopefully, providers will see many of the plans deciding to include these additional benefits in their MA bids to address the SDOH variables.
Additionally, in the Bipartisan Budget Act (BBA) that was passed in early 2018, Congress has taken it further by extending the lifting of the uniformity of the supplemental benefits to all chronically ill members of the MA plans effective January 1, 2020. This reinforces the need for us to gain valuable lessons during 2019 in order to determine what works and what doesn’t before it is transitioned to a broader population.
The Chronic Care Act of 2018 extended the Center for Medicare & Medicaid Innovation’s (CMMI) Valued-Based Insurance Design Model to all 50 states in 2020. This model was launched in 2017 to allow Medicare Advantage plans to offer supplemental benefits and reduced cost-sharing to seven conditions including Coronary Artery Disease or Congestive Heart Failure. The model focuses on four approaches:
- Reduced Cost Sharing for High-Value Services
- Reduced Cost Sharing for High-Value Providers
- Reduced Cost Sharing for enrollees participating in disease management
- Coverage of additional supplemental benefits such as transport or meal delivery
The creation of more supplemental benefits will enhance the quality of services we provide for our patients especially in terms of addressing the SDOH. Encouraging the inclusion of these targeted supplemental benefits will allow us to partner with payers to improve the health of the country in a more innovative way.
ADDRESSING SDOH WITH HEALTHCARE PROVIDERS AND COMMUNITY RESOURCES
At PCCI, we have been directly involved in national and state-driven education forums, presentations, and roundtables directed to design and deploy local models for the Connected Communities of Care program (previously known as the Information Exchange Portal) that bring together providers, payers, philanthropic organizations, community-based organizations (CBO), and local/state government entities. While most markets continue to be in a learning mode, significant and tangible activities are being initiated in a number of municipalities, including Dallas, Raleigh-Durham, Louisville, Detroit, Chicago, Phoenix, Salt Lake City, as well as across whole regions. For example, North Carolina recently requested proposals for the development of a North Carolina Resource Platform via the Foundation for Health Leadership & Innovation. The goal of this multi-year program is to connect over 3,000 statewide community-based organizations via technology, and facilitate SDOH. This will be completed through a programmatic coordination of referrals between healthcare providers and community resources to comprehensively identify and address the needs of individuals across the state. On a broader level, the Accountable Health Communities Model deployed in 2017 is engaging 31 organizations across the country to address a critical gap between clinical care and community services in the current healthcare delivery system. This is being done by testing the process of systematically identifying and addressing the health-related social needs of Medicare and Medicaid beneficiaries through screening, referral, and community navigation services to see if it will impact healthcare costs and reduce healthcare utilization.
SUCCESS IN SIX TRACKS
Our experience over the last five years across Dallas tells us that models will need to address six tracks to be successful: Governance, Legal, Technology, Clinical Workflows, CBO Workflows, and Sustainability (Figure 2). The maturity and evolution of the models need to develop and be staged within a multi-year deployment framework (concentric circles in Figure 2 represent the progression and evolution of the model with outer circles representing mature and more sophisticated models).

There is also a critical upfront readiness and deployment/implementation assessment that is important in order to stage the deployment of a Connected Community of Care program. This broad representation of the community’s fabric is critical to ensure that:
- A community is ready to undertake the operational and financial requirements associated with deploying a Connected Communities of Care program
- The healthcare and social needs of the community are at the forefront of the customized design of the platform (something most for-profit technology vendors offering an out-of-the-box solution either cannot do or fail to do properly)
- The design is sufficiently flexible to adjust as the healthcare or social needs of the community change
Addressing SDOH is finally moving from a “buzz” word to implementation pilots. While we talked a lot about population health over the last 10 years, doing population health without a truly engaged and “Connected Community of Care” is like focusing on rescuing people from drowning in a river vs. building a bridge so they can cross it safely. As we continue this journey, let us make sure we build a bridge that adapts to the needs of each community and has emerging local and national models of care to ensure sustainability. We don’t want to end up with a bridge like the Choluteca Bridge in Honduras, connecting nothing to nowhere.
Acknowledgments: Valinda Rutledge, PCCI Executive Advisor and Lindsey Nace, PCCI Marketing and Communications have contributed to this article.
Stay up-to-date with PCCI’s data science work by checking our recent news and follow us on Facebook, Twitter and LinkedIn!